
HALF A MILLION DOWNLOADS REACHED - Helping Safeguard children from psychiatric drug harm due to possible severe toxic side effects. We need alternatives like psychological interventions, physical activity, or mindfulness training as a first course of action. Let's 'Enable not Label' kids to give them better futures - - - - - - - - -"There can be no keener examination of a society's soul than the way it chooses to treat its children." - - - - - - Nelson Mandela
Popular Posts
-
Mindfulness is awareness of the present moment. It’s living here and now. Through mindfulness, you are freed from becoming entangled in tho...
-
Sir Ken Robinson's most watched YOUTUBE video disproves the medical 'epidemic' of ADHD IN THE U.S, Changing Educational P...
-
Does Technology Cause ADHD? Some experts believe that technology has a role in the rising rates of ADHD ; but whether it causes the disorde...
-
THE HPP MODEL OF MENTAL HEALTH AND WELLBEING FOR YOUNG PEOPLE FEATURES OF THE HPP MODEL - A multi-dimensional discursive appro...
-
"Mental Health issues are NOT disorders BUT a transient and often functional response to an accumulation of stressors in ...
-
At War With Ourselves Rufus May September 15, 2013 If we call someone mentally ill, in some ways we may b...
-
Will Self- author. Psychiatrists: the drug pushers Is the current epidemic of depression and hyperactivity the resu...
-
Prof Phillip Zimbardo Zimbardo Stanford Prison Experiment by Saul Mcleod, published 2008 Aim: To investigate how readily people wo...
-
Map of U.S. showing skewed prescription rate for ADHD - (low prescription use in west, with the sun and surf outlets, and higher across ...
-
The Great Dorothy Rowe on the DSM Manual http://www.ceimh.bham.ac.uk/tv/RowePart2.shtml WATCH THIS VERY POWERFUL CRITIQUE AND THEN SI...
Total Downloads Worldwide
Monday, 26 December 2011
Friday, 23 December 2011
ANTIPSYCHOTICS WITH 2 TO 5 YEAR OLDS DOUBLES IN 10 YEARS- COURTESY OF THE 'HealthDay' WEBSITE
More Toddlers, Young Children Given Antipsychotics
Researchers question the 'worrisome' trend.
MONDAY, Jan. 4 (HealthDay News) -- The rate of children aged 2 to 5 who are given antipsychotic medications has doubled in recent years, a new study has found.
Yet little is known about either the effectiveness or the safety of these powerful psychiatric medications in children this age, said researchers from Columbia University and Rutgers University, who looked at data on more than 1 million children with private health insurance.
"It is a worrisome trend, partly because very little is known about the short-term, let alone the long-term, safety of these drugs in this age group," said study author Dr. Mark Olfson, a professor of clinical psychiatry at Columbia University in New York City.
Prescribing antipsychotics to children in the upper range of that age span -- ages 4 and 5 -- is justifiable only in rare, intractable situations in which all other treatments, including family and psychological therapy, have been tried and are not working, Olfson said.
And it's questionable whether 2- and 3-year-olds should ever be prescribed antipsychotics, Olfson said.
The study is published in the January issue of the Journal of the American Academy of Child & Adolescent Psychiatry.
Presumably, only children with the most severe mental problems would be given the potent drugs. Yet, less than half of children on antipsychotics had received any mental health services, including a mental health assessment or treatment from a psychotherapist or psychiatrist, the study authors noted.
"You don't see the kinds of mental health services you would expect to see if we were dealing with the most profoundly disturbed toddlers," Olfson said, raising the question of whether doctors had done everything they could to help the child before turning to medications.
The overall numbers of children prescribed antipsychotics remains small, at less than one half of one percent of the national sample. But the numbers are rising. In 1999-2001, about one in 1,300 were being treated with antipsychotics. By 2007, that had risen to one in 630, according to Olfson.
For 5-year-olds, about one in 650 were being treated in 1999-2001. That doubled, to one in 329, in 2007, he noted.
Research published online in December in the journal Health Affairs by the same research team suggested children on Medicaid are even more likely than children with private insurance to be prescribed antipsychotics.
The most common antipsychotic drug prescribed to children was risperidone (Risperdal), which accounted for nearly three-quarters of antipsychotic prescriptions. In adults and teens, risperidone is used to treat schizophrenia and bipolar disorder. Risperidone is also approved by the U.S. Food and Drug Administration to treat unstable mood or irritability in children with autism aged 5 and up.
Children who were most likely to receive risperidone were male and aged 4 or 5, according to the report. The most common diagnosis was pervasive developmental disorder or mental retardation, attention deficit/hyperactivity disorder or disruptive behavior disorder.
Previous research has shown children on the drugs may experience metabolic and endocrine abnormalities. Little is known about their impact on the developing brain, Olfson added.
"I don't want to minimize the problems children can have at this age, but there are psychological treatments that have been proven to help parents and the kids that emphasize the quality of the parent-child relationship," Olfson said.
One reason for the uptick may be increasing numbers of children diagnosed with autism and some research showing risperidone may help with autism-related irritability, the researchers noted.
Dr. Peter Jensen, co-director of the division of child psychiatry and psychology at the Mayo Clinic, agreed that the trend is concerning. "We have no doubt there are prescribing practices out there that are very, very worrisome," Jensen said.
It's imperative that children receive a full mental health assessment before getting these drugs, to understand the family situation and school environment and if there is a family history of psychiatric problems, as well as undergoing a physical exam to rule out other medical problems.
"These agents should not be used as an adjunct to a family stressed to the max," Jensen said. "With kids who are 2 to 5, most can be managed without these medicines. Rarely a 5-year-old goes on them. But a child of 2 or 3, in my experience, I have never had to put them on [an antipsychotic]. There is so much else that can be done."
The stress and difficulty of coping with a child who has significant mental health issues, the need to have a child behave well enough to be permitted to attend school, as well as lack of adequate coverage for family therapy and mental health services, may push doctors and parents into believing they have little choice other than medicating the child, Jensen said.
More information
The U.S. National Mental Health Information Center has more on children and mental health issues.
SOURCES: Mark Olfson, M.D., M.P.H., professor, clinical psychiatry, Columbia University, New York City; Peter Jensen, M.D., co-director, division of child psychiatry and psychology, Mayo Clinic, Rochester, Minn.; January 2010, Journal of the American Academy of Child & Adolescent Psychiatry
YOUNGEST CHILDREN IN YEAR GROUP REGULARLY DIAGNOSED WITH ADHD FOR SHOWING IMMATURE BEHAVIOUR RELATIVE TO PEERS - NOT SURPRISING REALLY
 | |
| TIDAL WAVE OF ADHD DIAGNOSES HITS U.K. |
One million children misdiagnosed with ADHD
Wednesday, December 01, 2010 by: Monica G. Young
See all articles by this author
Email this author
(NaturalNews) Nearly 1 million U.S. children are potentially misdiagnosed with ADHD simply because they are the youngest in their class, according to a recent study by a Michigan State University economist, Todd Elder.
Using a sampling of about 12,000 children, he compared ADHD diagnosis and medication rates between the youngest and oldest in each grade. Elder found the youngest kindergartners (typically less mature) were 60 percent more likely to be diagnosed with ADHD than the oldest in that grade. And by the time students reached the fifth to eighth grades, the youngest were more than twice as likely to be prescribed stimulants.
"If a child is behaving poorly, if he's inattentive, if he can't sit still, it may simply be because he's 5 and the other kids are 6," said Elder, assistant professor of economics. "Many ADHD diagnoses may be driven by teachers' perceptions of poor behavior among the youngest children in a kindergarten classroom."
He pointed out that although teachers cannot diagnose ADHD, their opinions are instrumental in decisions to send a child for a mental health evaluation.
This study suggests that 20 percent - or 900,000 - of the 4.5 million children currently labeled with ADHD have been misdiagnosed based on their age relative to classmates.
No blood tests or other medical analyses are used in diagnosing ADHD (Attention Deficit Hyperactivity Disorder). Children so labeled are routinely prescribed high-risk psychostimulants, despite documented adverse effects that can range from loss of appetite, anxiety and insomnia to stunted growth, high blood pressure and heart failure.
In 1987, the American Psychiatric Association voted ADHD into the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders 4th edition - the psychiatric bible used in prescribing medication) as an authorized "mental disorder". There was no scientific evidence to support this as a brain malfunction, disease, chemical imbalance or neuro-biological condition. Yet psychostimulants widely prescribed for ADHD alter the natural chemistry of the brain and body and can have long term impact on children's health.
Big Pharma spends billions in convincing the public, schools, legislators and the press that ADHD, ADD and other so-called mental disorders are diseases on par with verifiable medical conditions such as diabetes and heart disease.
How could all this come to be? The ADHD myth and its costly medications bring the pharmaceutical and psychiatric industries billions of dollars a year in revenue.
This marketing deception is not isolated to the U.S. A recent Canadian study suggests that many boys are prescribed ADHD drugs for being, well, boys. (Core symptoms used in diagnoses are inability to focus and hyper and impulsive behavior.) On Oct 18, 2010 Canada's Globe and Mail published an article entitled "Are we medicating a disorder or treating boyhood as a disease?"
"Last year, more than two million prescriptions for Ritalin and other ADHD drugs were written specifically for children under 17, and at least 75 per cent of them were for young males", wrote the author. The Globe's investigation shows that prescriptions for ADHD drugs in Canada shot up to 2.9 million in 2009, a jump of more than 55 per cent in four years. And ADHD prescriptions for males increased 50 per cent since 2005.
Sources for this story include:
http://news.msu.edu/story/8160/
http://www.cchrint.org/2010/10/30/1...
http://www.theglobeandmail.com/news...
http://www.adhdtesting.org/
About the author
Monica G. Young is a lifelong advocate for human rights. She is an educational researcher and writer with a purpose to expose the truth about the pharmaceutical and psychiatric industries. She encourages non-drug alternative approaches based on healthy lifestyles and human decency.
Learn more: http://www.naturalnews.com/030580_ADHD_children.html#ixzz1hOUNWqNm
DSM5 - THE ROUTES TO MORE DRUG DEPENDENCY FOR KIDS.
Psychologists' DSM5 Petition Catching like Wildfire -
Grassroots campaign generating blaze of interest.
Published on October 27, 2011 by Karen Franklin, Ph.D. in Witness
An online petition by psychologists concerned about the lack of science underlying proposed changes in the American Psychiatric Association's Diagnostic and Statistical Manual (DSM) is taking off like wildfire, with more than 1,100 signatures as of this morning.
The blaze of interest is especially remarkable because the petition was launched without any publicity at all, and has gained traction solely through word of mouth.
The coalition of psychologists is publicly urging the American Psychiatric Association to reconsider the mental illness expansions and biomedical emphasis proposed for the fifth edition of the DSM, due out in 2013. The DSM-5 will reify disorders with little empirical support, lower the threshold for mental disorder, and foreground a purely biological approach to mental illness.
Related Articles
Why Doesn't DSM 5 Defend Itself?
DSM-5 Task Force Extends Deadline for Sending Comments
DSM 5 Needs An Independent Scientific Review
The User's Revolt Against DSM 5
What Would a Useful DSM 5 Look Like?
The coalition's online petitition comes on the heels of a similar public statement by the British Psychological Society, which I blogged about back in June.
The petition coalition expresses grave concern about the overemphasis on biomedical explanations for mental health problems, and the resulting overprescribing of dangerous psychiatric drugs:
In the absence of compelling evidence, we are concerned that these reconceptualizations of mental disorder as primarily medical phenomena may have scientific, socioeconomic, and forensic consequences....
Taken together, these proposed changes seem to depart from DSM's 30-year "atheoretical" stance in favor of a pathophysiological model. This move appears to overlook growing disenchantment with strict neurobiological theories of mental disorder (e.g., "chemical imbalance" theories such as the dopamine theory of schizophrenia and the serotonin theory of depression), as well as the general failure of the neo-Kraepelinian model for validating psychiatric illness....
We thus believe that a move towards biological theory directly contradicts evidence that psychopathology, unlike medical pathology, cannot be reduced to pathognomonic physiological signs or even multiple biomarkers. Further, growing evidence suggests that though psychotropic medications do not necessarily correct putative chemical imbalances, they do pose substantial iatrogenic hazards. For example, the increasingly popular neuroleptic (antipsychotic) medications, though helpful for many people in the short term, pose the long-term risks of obesity, diabetes, movement disorders, cognitive decline, worsening of psychotic symptoms, reduction in brain volume, and shortened lifespan.
Allen Frances, who chaired the task force of the previous DSM, the DSM-IV, and has been openly critical of the current process, said in an article in yesterday's Psychiatric Times that the APA plans no official response:
They hope to ride out the storm of opposition mounting on all sides and dismiss it as the work of professional rivals or antipsychiatry malcontents. Characteristically, DSM-5 offers no rebuttal based on evidence. Instead, it stubbornly soldiers on in its promotion of radical diagnostic changes that are risky, untested, unsupported by a strong science base, and vigorously opposed by the field.
Frances has another good commentary on the petition and its ramifications at his Psychology Today blog, DSM5 in Distress:
DSM 5 has lived in a world that seems to be hermetically sealed. Despite the obvious impossibility of many of its proposals, it shows no ability to self correct or learn from outside advice. The current drafts have changed almost not at all from their deeply flawed originals. The DSM 5 field trials ask the wrong questions and will make no contribution to the endgame.
But the DSM 5 deafness may finally be cured by a users' revolt. The APA budget depends heavily on the huge publishing profits that accrue from its DSM sales. APA has ignored the scientific, clinical, and public health reasons it should omit the most dangerous suggestions- but I suspect APA will be more sensitive to the looming risk of a boycott by users.
I encourage readers to view and sign this important petition, by clicking on the link below. You can also email the petition to others. So, spread the word.
CLICK HERE TO VISIT THE PETITION SITE.
DSM5 COUNTDOWN TO 2013 - NEW YORK TIMES ARTICLE HIGHLIGHTS SOME OF THE RISKS TO OUR CHILDREN
Revising Book on Disorders of the Mind.
By BENEDICT CAREY
Published: February 10, 2010
Far fewer children would get a diagnosis of bipolar disorder. “Binge eating disorder” and “hypersexuality” might become part of the everyday language. And the way many mental disorders are diagnosed and treated would be sharply revised.
Multimedia
Rethinking Personality DisordersGraphic
Rethinking Personality Disorders
Readers’ Comments
"Definitions of mental disorders will always be controversial. Human behavior and the functioning of the brain are simply too complex to put in boxes with neat labels."
These are a few of the changes proposed on Tuesday by doctors charged with revising psychiatry’s encyclopedia of mental disorders, the guidebook that largely determines where society draws the line between normal and not normal, between eccentricity and illness, between self-indulgence and self-destruction — and, by extension, when and how patients should be treated.
The eagerly awaited revisions — to be published, if adopted, in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, due in 2013 — would be the first in a decade.
For months they have been the subject of intense speculation and lobbying by advocacy groups, and some proposed changes have already been widely discussed — including folding the diagnosis of Asperger’s syndrome into a broader category, autism spectrum disorder.
But others, including a proposed alternative for bipolar disorder in many children, were unveiled on Tuesday. Experts said the recommendations, posted online at DSM5.org for public comment, could bring rapid change in several areas.
“Anything you put in that book, any little change you make, has huge implications not only for psychiatry but for pharmaceutical marketing, research, for the legal system, for who’s considered to be normal or not, for who’s considered disabled,” said Dr. Michael First, a professor of psychiatry at Columbia University who edited the fourth edition of the manual but is not involved in the fifth.
“And it has huge implications for stigma,” Dr. First continued, “because the more disorders you put in, the more people get labels, and the higher the risk that some get inappropriate treatment.”
One significant change would be adding a childhood disorder called temper dysregulation disorder with dysphoria, a recommendation that grew out of recent findings that many wildly aggressive, irritable children who have been given a diagnosis of bipolar disorder do not have it.
The misdiagnosis led many children to be given powerful antipsychotic drugs, which have serious side effects, including metabolic changes.
“The treatment of bipolar disorder is meds first, meds second and meds third,” said Dr. Jack McClellan, a psychiatrist at the University of Washington who is not working on the manual. “Whereas if these kids have a behavior disorder, then behavioral treatment should be considered the primary treatment.”
Some diagnoses of bipolar disorder have been in children as young as 2, and there have been widespread reports that doctors promoting the diagnosis received consulting and speaking fees from the makers of the drugs.
In a conference call on Tuesday, Dr. David Shaffer, a child psychiatrist at Columbia, said he and his colleagues on the panel working on the manual “wanted to come up with a diagnosis that captures the behavioral disturbance and mood upset, and hope the people contemplating a diagnosis of bipolar for these patients would think again.”
Experts gave the American Psychiatric Association, which publishes the manual, predictably mixed reviews. Some were relieved that the task force working on the manual — which includes neurologists and psychologists as well as psychiatrists — had revised the previous version rather than trying to rewrite it.
Others criticized the authors, saying many diagnoses in the manual would still lack a rigorous scientific basis.
The good news, said Edward Shorter, a historian of psychiatry who has been critical of the manual, is that most patients will be spared the confusion of a changed diagnosis. But “the bad news,” he added, “is that the scientific status of the main diseases in previous editions of the D.S.M. — the keystones of the vault of psychiatry — is fragile.”
To more completely characterize all patients, the authors propose using measures of severity, from mild to severe, and ratings of symptoms, like anxiety, that are found as often with personality disorders as with depression.
“In the current version of the manual, people either meet the threshold by having a certain number of symptoms, or they don’t,” said Dr. Darrel A. Regier, the psychiatric association’s research director and, with Dr. David J. Kupfer of the University of Pittsburgh, the co-chairman of the task force. “But often that doesn’t fit reality. Someone with schizophrenia might have symptoms of insomnia, of anxiety; these aren’t the diagnostic criteria for schizophrenia, but they affect the patient’s life, and we’d like to have a standard way of measuring them.”
In a conference call on Tuesday, Dr. Regier, Dr. Kupfer and several other members of the task force outlined their favored revisions. The task force favored making semantic changes that some psychiatrists have long argued for, trading the term “mental retardation” for “intellectual disability,” for instance, and “substance abuse” for “addiction.”
One of the most controversial proposals was to identify “risk syndromes,” that is, a risk of developing a disorder like schizophrenia or dementia. Studies of teenagers identified as at high risk of developing psychosis, for instance, find that 70 percent or more in fact do not come down with the disorder.
“I completely understand the idea of trying to catch something early,” Dr. First said, “but there’s a huge potential that many unusual, semi-deviant, creative kids could fall under this umbrella and carry this label for the rest of their lives.”
Dr. William T. Carpenter, a psychiatrist at the University of Maryland and part of the group proposing the idea, said it needed more testing. “Concerns about stigma and excessive treatment must be there,” he said. “But keep in mind that these are individuals seeking help, who have distress, and the question is, What’s wrong with them?”
The panel proposed adding several disorders with a high likelihood of entering the pop vernacular. One, a new description of sex addiction, is “hypersexuality,” which, in part, is when “a great deal of time is consumed by sexual fantasies and urges; and in planning for and engaging in sexual behavior.”
Another is “binge eating disorder,” defined as at least one binge a week for three months — eating platefuls of food, fast, and to the point of discomfort — accompanied by severe guilt and plunges in mood.
“This is not the normative overeating that we all do, by any means,” said Dr. B. Timothy Walsh, a psychiatrist at Columbia and the New York State Psychiatric Institute who is working on the manual. “It involves much more loss of control, more distress, deeper feelings of guilt and unhappiness.”
A version of this article appeared in print on February 10, 2010, on page A1 of the New York edition.
FOODS WHICH INCREASE RISKS OF ADHD SYMPTOMS
For years, doctors have speculated that certain foods may play a role in ADHD. Although much research has been done on the subject, it’s still not believed that food actually causes ADHD. What diet does seem do, however, is worsen ADHD symptoms or trigger symptoms that mimic the signs of ADHD in children. “Excessive caffeine and excessive use of fast foods and other foods of poor nutritional value can cause kids to display behavior that might be confused with ADHD,” says Frank Barnhill, MD, an expert on ADHD and the author of Mistaken for ADHD. The following foods in particular have been implicated in ADHD in one way or another.
Candy
Candy is loaded with sugar and artificial colors, which is a bad combination when it comes to children with ADHD who often need to follow an ADHD diet. Both of these components have been shown to promote ADHD symptoms in studies. “With the high content of sugar and artificial coloring, candy is a huge contributor to ADHD,” says Howard Peiper, author of The ADD and ADH
Soda
If you have ADHD, consider eliminating soda. These sweet drinks often have many of the same sugars and sweeteners that make candy a bad idea for kids on the ADHD diet. Soda also has other ingredients that can help worsen ADHD symptoms, such as high-fructose corn syrup and caffeine. “Excessive sugar and caffeine intake both cause symptoms of hyperactivity and easy distractibility,” says Dr. Barnhill.
Cake Mixes and Frostings
Cake mix and frosting contain the high amounts of sugar and artificial colors that can lead to hyperactivity and other ADHD symptoms. Naheed Ali, MD, ADHD expert and the author of Diabetes and You: A Comprehensive, Holistic Approach, adds that these products are often also loaded with several artificial sweeteners. “When frosting and cake mix contain artificial sweeteners, they increase the risk of ADHD symptoms more than natural sweeteners would,” he says.
Energy Drinks
Energy drinks are becoming increasingly popular among kids, especially teens. Unfortunately, they also have a veritable treasure trove of ingredients that can worsen ADHD symptoms: sugar, artificial sweeteners, artificial colors, caffeine, and other stimulants. “Energy drinks are high on the list of things that cause teens to display behaviors mimicking ADHD,” says Barnhill. They have no place in a healthy ADHD diet.
Frozen Fruits and Vegetables
Most fruits and vegetables are healthy choices for an ADHD diet, but some frozen varieties can contain artificial colors, so check all labels carefully. Barnhill says these can cause ADHD symptoms for another reason as well. “Foods treated with organophosphates for insect control have been shown to cause neurologic-based behavioral problems that mimic ADHD and many other behavior problems,” he say
Fish and Other Seafood
Dr. Ali says that eating fish and other seafood with trace amounts of mercury can cause ADHD symptoms in the long term. Some of the worst culprits are shark, king mackerel, swordfish, and tilefish. “Mercury, like cellulose, is extremely hard to digest and can accumulate in the brain over time,” explains Ali. “This can lead to hyperactivity.” Talk to your doctor or ADHD nutritionist about the best types of fish to include in your ADHD diet.
Other Food Sensitivities
According to a recent study, many children with food sensitivities can exhibit ADHD symptoms after they are exposed to certain foods. Based on the results of the research, some of the common foods that can cause ADHD reactions include milk, chocolate, soy, wheat, eggs, beans, corn, tomatoes, grapes, and oranges. If you suspect a food sensitivity may be contributing to your child’s ADHD symptoms, talk to your doctor about the possibility of trying an elimination diet.
MARCIA ANGELL - "DRUG COMPANIES AND DOCTORS - A STORY OF CORRUPTION." ARTICLE AND VIDEO
Drug Companies & Doctors:
A Story of Corruption
By MARCIA ANGELL
http://youtu.be/kWLQpnRlt5A 
WATCH THIS EXCELLENT VIDEO ABOUT THIS MORAL QUESTION OF OUR TIME.
Marcia Angell is a Senior Lecturer in Social Medicine at Harvard Medical School. A physician, she is a former Editor in Chief of the highly prestigious New England Journal of Medicine. Her latest book is The Truth About the Drug Companies: How They Deceive Us and What to Do About It. (January 2009)
Recently Senator Charles Grassley, ranking Republican on the Senate Finance Committee, has been looking into financial ties between the pharmaceutical industry and the academic physicians who largely determine the market value of prescription drugs. He hasn't had to look very hard.Take the case of Dr. Joseph L. Biederman, professor of psychiatry at Harvard Medical School and chief of pediatric psychopharmacology at Harvard's Massachusetts General Hospital. Thanks largely to him, children as young as two years old are now being diagnosed with bipolar disorder and treated with a cocktail of powerful drugs, many of which were not approved by the Food and Drug Administration (FDA) for that purpose and none of which were approved for children below ten years of age.
Legally, physicians may use drugs that have already been approved for a particular purpose for any other purpose they choose, but such use should be based on good published scientific evidence. That seems not to be the case here. Biederman's own studies of the drugs he advocates to treat childhood bipolar disorder were, as The New York Times summarized the opinions of its expert sources, "so small and loosely designed that they were largely inconclusive."[1]
In June, Senator Grassley revealed that drug companies, including those that make drugs he advocates for childhood bipolar disorder, had paid Biederman $1.6 million in consulting and speaking fees between 2000 and 2007. Two of his colleagues received similar amounts. After the revelation, the president of the Massachusetts General Hospital and the chairman of its physician organization sent a letter to the hospital's physicians expressing not shock over the enormity of the conflicts of interest, but sympathy for the beneficiaries: "We know this is an incredibly painful time for these doctors and their families, and our hearts go out to them."
Or consider Dr. Alan F. Schatzberg, chair of Stanford's psychiatry department and president-elect of the American Psychiatric Association. Senator Grassley found that Schatzberg controlled more than $6 million worth of stock in Corcept Therapeutics, a company he cofounded that is testing mifepristone—the abortion drug otherwise known as RU-486—as a treatment for psychotic depression. At the same time, Schatzberg was the principal investigator on a National Institute of Mental Health grant that included research on mifepristone for this use and he was coauthor of three papers on the subject. In a statement released in late June, Stanford professed to see nothing amiss in this arrangement, although a month later, the university's counsel announced that it was temporarily replacing Schatzberg as principal investigator "to eliminate any misunderstanding."
Perhaps the most egregious case exposed so far by Senator Grassley is that of Dr. Charles B. Nemeroff, chair of Emory University's department of psychiatry and, along with Schatzberg, coeditor of the influential Textbook of Psychopharmacology.[2] Nemeroff was the principal investigator on a five-year $3.95 million National Institute of Mental Health grant—of which $1.35 million went to Emory for overhead—to study several drugs made by GlaxoSmithKline. To comply with university and government regulations, he was required to disclose to Emory income from GlaxoSmithKline, and Emory was required to report amounts over $10,000 per year to the National Institutes of Health, along with assurances that the conflict of interest would be managed or eliminated.
But according to Senator Grassley, who compared Emory's records with those from the company, Nemeroff failed to disclose approximately $500,000 he received from GlaxoSmithKline for giving dozens of talks promoting the company's drugs. In June 2004, a year into the grant, Emory conducted its own investigation of Nemeroff's activities, and found multiple violations of its policies. Nemeroff responded by assuring Emory in a memorandum, "In view of the NIMH/Emory/GSK grant, I shall limit my consulting to GSK to under $10,000/year and I have informed GSK of this policy." Yet that same year, he received $171,031 from the company, while he reported to Emory just $9,999—a dollar shy of the $10,000 threshold for reporting to the National Institutes of Health.
Emory benefited from Nemeroff's grants and other activities, and that raises the question of whether its lax oversight was influenced by its own conflicts of interest. As reported by Gardiner Harris in TheNew York Times,[3] Nemeroff himself had pointed out his value to Emory in a 2000 letter to the dean of the medical school, in which he justified his membership on a dozen corporate advisory boards by saying:
Surely you remember that Smith-Kline Beecham Pharmaceuticals donated an endowed chair to the department and there is some reasonable likelihood that Janssen Pharmaceuticals will do so as well. In addition, Wyeth-Ayerst Pharmaceuticals has funded a Research Career Development Award program in the department, and I have asked both AstraZeneca Pharmaceuticals and Bristol-Meyers [sic] Squibb to do the same. Part of the rationale for their funding our faculty in such a manner would be my service on these boards.Because these psychiatrists were singled out by Senator Grassley, they received a great deal of attention in the press, but similar conflicts of interest pervade medicine. (The senator is now turning his attention to cardiologists.) Indeed, most doctors take money or gifts from drug companies in one way or another. Many are paid consultants, speakers at company-sponsored meetings, ghost-authors of papers written by drug companies or their agents[4] and ostensible "researchers" whose contribution often consists merely of putting their patients on a drug and transmitting some token information to the company. Still more doctors are recipients of free meals and other out-and-out gifts. In addition, drug companies subsidize most meetings of professional organizations and most of the continuing medical education needed by doctors to maintain their state licenses.
No one knows the total amount provided by drug companies to physicians, but I estimate from the annual reports of the top nine US drug companies that it comes to tens of billions of dollars a year. By such means, the pharmaceutical industry has gained enormous control over how doctors evaluate and use its own products. Its extensive ties to physicians, particularly senior faculty at prestigious medical schools, affect the results of research, the way medicine is practiced, and even the definition of what constitutes a disease.
Consider the clinical trials by which drugs are tested in human subjects.[5] Before a new drug can enter the market, its manufacturer must sponsor clinical trials to show the Food and Drug Administration that the drug is safe and effective, usually as compared with a placebo or dummy pill. The results of all the trials (there may be many) are submitted to the FDA, and if one or two trials are positive—that is, they show effectiveness without serious risk—the drug is usually approved, even if all the other trials are negative. Drugs are approved only for a specified use—for example, to treat lung cancer—and it is illegal for companies to promote them for any other use.
But physicians may prescribe approved drugs "off label"—i.e., without regard to the specified use—and perhaps as many as half of all prescriptions are written for off-label purposes. After drugs are on the market, companies continue to sponsor clinical trials, sometimes to get FDA approval for additional uses, sometimes to demonstrate an advantage over competitors, and often just as an excuse to get physicians to prescribe such drugs for patients. (Such trials are aptly called "seeding" studies.)
Since drug companies don't have direct access to human subjects, they need to outsource their clinical trials to medical schools, where researchers use patients from teaching hospitals and clinics, or to private research companies (CROs), which organize office-based physicians to enroll their patients. Although CROs are usually faster, sponsors often prefer using medical schools, in part because the research is taken more seriously, but mainly because it gives them access to highly influential faculty physicians—referred to by the industry as "thought-leaders" or "key opinion leaders" (KOLs). These are the people who write textbooks and medical journal papers, issue practice guidelines (treatment recommendations), sit on FDA and other governmental advisory panels, head professional societies, and speak at the innumerable meetings and dinners that take place every year to teach clinicians about prescription drugs. Having KOLs like Dr. Biederman on the payroll is worth every penny spent.
A few decades ago, medical schools did not have extensive financial dealings with industry, and faculty investigators who carried out industry-sponsored research generally did not have other ties to their sponsors. But schools now have their own manifold deals with industry and are hardly in a moral position to object to their faculty behaving in the same way. A recent survey found that about two thirds of academic medical centers hold equity interest in companies that sponsor research within the same institution.[6] A study of medical school department chairs found that two thirds received departmental income from drug companies and three fifths received personal income.[7] In the 1980s medical schools began to issue guidelines governing faculty conflicts of interest but they are highly variable, generally quite permissive, and loosely enforced.
Because drug companies insist as a condition of providing funding that they be intimately involved in all aspects of the research they sponsor, they can easily introduce bias in order to make their drugs look better and safer than they are. Before the 1980s, they generally gave faculty investigators total responsibility for the conduct of the work, but now company employees or their agents often design the studies, perform the analysis, write the papers, and decide whether and in what form to publish the results. Sometimes the medical faculty who serve as investigators are little more than hired hands, supplying patients and collecting data according to instructions from the company.
In view of this control and the conflicts of interest that permeate the enterprise, it is not surprising that industry-sponsored trials published in medical journals consistently favor sponsors' drugs—largely because negative results are not published, positive results are repeatedly published in slightly different forms, and a positive spin is put on even negative results. A review of seventy-four clinical trials of antidepressants, for example, found that thirty-seven of thirty-eight positive studies were published.[8] But of the thirty-six negative studies, thirty-three were either not published or published in a form that conveyed a positive outcome. It is not unusual for a published paper to shift the focus from the drug's intended effect to a secondary effect that seems more favorable.
The suppression of unfavorable research is the subject of Alison Bass's engrossing book, Side Effects: A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial. This is the story of how the British drug giant GlaxoSmithKline buried evidence that its top-selling antidepressant, Paxil, was ineffective and possibly harmful to children and adolescents. Bass, formerly a reporter for the Boston Globe, describes the involvement of three people—a skeptical academic psychiatrist, a morally outraged assistant administrator in Brown University's department of psychiatry (whose chairman received in 1998 over $500,000 in consulting fees from drug companies, including GlaxoSmithKline), and an indefatigable New York assistant attorney general. They took on GlaxoSmithKline and part of the psychiatry establishment and eventually prevailed against the odds.
The book follows the individual struggles of these three people over many years, culminating with GlaxoSmithKline finally agreeing in 2004 to settle charges of consumer fraud for $2.5 million (a tiny fraction of the more than $2.7 billion in yearly Paxil sales about that time). It also promised to release summaries of all clinical trials completed after December 27, 2000. Of much greater significance was the attention called to the deliberate, systematic practice of suppressing unfavorable research results, which would never have been revealed without the legal discovery process. Previously undisclosed, one of GlaxoSmithKline's internal documents said, "It would be commercially unacceptable to include a statement that efficacy had not been demonstrated, as this would undermine the profile of paroxetine [Paxil]."[9]
Many drugs that are assumed to be effective are probably little better than placebos, but there is no way to know because negative results are hidden. One clue was provided six years ago by four researchers who, using the Freedom of Information Act, obtained FDA reviews of every placebo-controlled clinical trial submitted for initial approval of the six most widely used antidepressant drugs approved between 1987 and 1999—Prozac, Paxil, Zoloft, Celexa, Serzone, and Effexor.[10] They found that on average, placebos were 80 percent as effective as the drugs. The difference between drug and placebo was so small that it was unlikely to be of any clinical significance. The results were much the same for all six drugs: all were equally ineffective. But because favorable results were published and unfavorable results buried (in this case, within the FDA), the public and the medical profession believed these drugs were potent antidepressants.
Clinical trials are also biased through designs for research that are chosen to yield favorable results for sponsors. For example, the sponsor's drug may be compared with another drug administered at a dose so low that the sponsor's drug looks more powerful. Or a drug that is likely to be used by older people will be tested in young people, so that side effects are less likely to emerge. A common form of bias stems from the standard practice of comparing a new drug with a placebo, when the relevant question is how it compares with an existing drug. In short, it is often possible to make clinical trials come out pretty much any way you want, which is why it's so important that investigators be truly disinterested in the outcome of their work.
Conflicts of interest affect more than research. They also directly shape the way medicine is practiced, through their influence on practice guidelines issued by professional and governmental bodies, and through their effects on FDA decisions. A few examples: in a survey of two hundred expert panels that issued practice guidelines, one third of the panel members acknowledged that they had some financial interest in the drugs they considered.[11] In 2004, after the National Cholesterol Education Program called for sharply lowering the desired levels of "bad" cholesterol, it was revealed that eight of nine members of the panel writing the recommendations had financial ties to the makers of cholesterol-lowering drugs.[12] Of the 170 contributors to the most recent edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM), ninety-five had financial ties to drug companies, including all of the contributors to the sections on mood disorders and schizophrenia.[13] Perhaps most important, many members of the standing committees of experts that advise the FDA on drug approvals also have financial ties to the pharmaceutical industry.[14]
In recent years, drug companies have perfected a new and highly effective method to expand their markets. Instead of promoting drugs to treat diseases, they have begun to promote diseases to fit their drugs. The strategy is to convince as many people as possible (along with their doctors, of course) that they have medical conditions that require long-term drug treatment. Sometimes called "disease-mongering," this is a focus of two new books: Melody Petersen's Our Daily Meds: How the Pharmaceutical Companies Transformed Themselves into Slick Marketing Machines and Hooked the Nation on Prescription Drugs and Christopher Lane's Shyness: How Normal Behavior Became a Sickness.
To promote new or exaggerated conditions, companies give them serious-sounding names along with abbreviations. Thus, heartburn is now "gastro-esophageal reflux disease" or GERD; impotence is "erectile dysfunction" or ED; premenstrual tension is "premenstrual dysphoric disorder" or PMDD; and shyness is "social anxiety disorder" (no abbreviation yet). Note that these are ill-defined chronic conditions that affect essentially normal people, so the market is huge and easily expanded. For example, a senior marketing executive advised sales representatives on how to expand the use of Neurontin: "Neurontin for pain, Neurontin for monotherapy, Neurontin for bipolar, Neurontin for everything."[15] It seems that the strategy of the drug marketers—and it has been remarkably successful—is to convince Americans that there are only two kinds of people: those with medical conditions that require drug treatment and those who don't know it yet. While the strategy originated in the industry, it could not be implemented without the complicity of the medical profession.
Melody Petersen, who was a reporter for The New York Times, has written a broad, convincing indictment of the pharmaceutical industry.[16] She lays out in detail the many ways, both legal and illegal, that drug companies can create "blockbusters" (drugs with yearly sales of over a billion dollars) and the essential role that KOLs play. Her main example is Neurontin, which was initially approved only for a very narrow use—to treat epilepsy when other drugs failed to control seizures. By paying academic experts to put their names on articles extolling Neurontin for other uses—bipolar disease, post-traumatic stress disorder, insomnia, restless legs syndrome, hot flashes, migraines, tension headaches, and more—and by funding conferences at which these uses were promoted, the manufacturer was able to parlay the drug into a blockbuster, with sales of $2.7 billion in 2003. The following year, in a case covered extensively by Petersen for the Times, Pfizer pleaded guilty to illegal marketing and agreed to pay $430 million to resolve the criminal and civil charges against it. A lot of money, but for Pfizer, it was just the cost of doing business, and well worth it because Neurontin continued to be used like an all-purpose tonic, generating billions of dollars in annual sales.
Christopher Lane's book has a narrower focus—the rapid increase in the number of psychiatric diagnoses in the American population and in the use of psychoactive drugs (drugs that affect mental states) to treat them. Since there are no objective tests for mental illness and the boundaries between normal and abnormal are often uncertain, psychiatry is a particularly fertile field for creating new diagnoses or broadening old ones.[17] Diagnostic criteria are pretty much the exclusive province of the current edition of the Diagnostic and Statistical Manual of Mental Disorders, which is the product of a panel of psychiatrists, most of whom, as I mentioned earlier, had financial ties to the pharmaceutical industry. Lane, a research professor of literature at Northwestern University, traces the evolution of the DSM from its modest beginnings in 1952 as a small, spiral-bound handbook (DSM-I) to its current 943-page incarnation (the revised version of DSM-IV) as the undisputed "bible" of psychiatry—the standard reference for courts, prisons, schools, insurance companies, emergency rooms, doctors' offices, and medical facilities of all kinds.
Given its importance, you might think that the DSM represents the authoritative distillation of a large body of scientific evidence. But Lane, using unpublished records from the archives of the American Psychiatric Association and interviews with the princi-pals, shows that it is instead the product of a complex of academic politics, personal ambition, ideology, and, perhaps most important, the influence of the pharmaceutical industry. What the DSM lacks is evidence. Lane quotes one contributor to the DSM-III task force:
There was very little systematic research, and much of the research that existed was really a hodgepodge—scattered, inconsistent, and ambiguous. I think the majority of us recognized that the amount of good, solid science upon which we were making our decisions was pretty modest.Lane uses shyness as his case study of disease-mongering in psychiatry. Shyness as a psychiatric illness made its debut as "social phobia" in DSM-III in 1980, but was said to be rare. By 1994, when DSM-IV was published, it had become "social anxiety disorder," now said to be extremely common. According to Lane, GlaxoSmithKline, hoping to boost sales for its antidepressant, Paxil, decided to promote social anxiety disorder as "a severe medical condition." In 1999, the company received FDA approval to market the drug for social anxiety disorder. It launched an extensive media campaign to do it, including posters in bus shelters across the country showing forlorn individuals and the words "Imagine being allergic to people...," and sales soared. Barry Brand, Paxil's product director, was quoted as saying, "Every marketer's dream is to find an unidentified or unknown market and develop it. That's what we were able to do with social anxiety disorder."
Some of the biggest blockbusters are psychoactive drugs. The theory that psychiatric conditions stem from a biochemical imbalance is used as a justification for their widespread use, even though the theory has yet to be proved. Children are particularly vulnerable targets. What parents dare say "No" when a physician says their difficult child is sick and recommends drug treatment? We are now in the midst of an apparent epidemic of bipolar disease in children (which seems to be replacing attention-deficit hyperactivity disorder as the most publicized condition in childhood), with a forty-fold increase in the diagnosis between 1994 and 2003.[18] These children are often treated with multiple drugs off-label, many of which, whatever their other properties, are sedating, and nearly all of which have potentially serious side effects.
The problems I've discussed are not limited to psychiatry, although they reach their most florid form there. Similar conflicts of interest and biases exist in virtually every field of medicine, particularly those that rely heavily on drugs or devices. It is simply no longer possible to believe much of the clinical research that is published, or to rely on the judgment of trusted physicians or authoritative medical guidelines. I take no pleasure in this conclusion, which I reached slowly and reluctantly over my two decades as an editor of The New England Journal of Medicine.
One result of the pervasive bias is that physicians learn to practice a very drug-intensive style of medicine. Even when changes in lifestyle would be more effective, doctors and their patients often believe that for every ailment and discontent there is a drug. Physicians are also led to believe that the newest, most expensive brand-name drugs are superior to older drugs or generics, even though there is seldom any evidence to that effect because sponsors do not usually compare their drugs with older drugs at equivalent doses. In addition, physicians, swayed by prestigious medical school faculty, learn to prescribe drugs for off-label uses without good evidence of effectiveness.
It is easy to fault drug companies for this situation, and they certainly deserve a great deal of blame. Most of the big drug companies have settled charges of fraud, off-label marketing, and other offenses. TAP Pharmaceuticals, for example, in 2001 pleaded guilty and agreed to pay $875 million to settle criminal and civil charges brought under the federal False Claims Act over its fraudulent marketing of Lupron, a drug used for treatment of prostate cancer. In addition to GlaxoSmithKline, Pfizer, and TAP, other companies that have settled charges of fraud include Merck, Eli Lilly, and Abbott. The costs, while enormous in some cases, are still dwarfed by the profits generated by these illegal activities, and are therefore not much of a deterrent. Still, apologists might argue that the pharmaceutical industry is merely trying to do its primary job—further the interests of its investors—and sometimes it goes a little too far.
Physicians, medical schools, and professional organizations have no such excuse, since their only fiduciary responsibility is to patients. The mission of medical schools and teaching hospitals—and what justifies their tax-exempt status—is to educate the next generation of physicians, carry out scientifically important research, and care for the sickest members of society. It is not to enter into lucrative commercial alliances with the pharmaceutical industry. As reprehensible as many industry practices are, I believe the behavior of much of the medical profession is even more culpable.[19] Drug companies are not charities; they expect something in return for the money they spend, and they evidently get it or they wouldn't keep paying.
So many reforms would be necessary to restore integrity to clinical research and medical practice that they cannot be summarized briefly. Many would involve congressional legislation and changes in the FDA, including its drug approval process. But there is clearly also a need for the medical profession to wean itself from industry money almost entirely. Although industry–academic collaboration can make important scientific contributions, it is usually in carrying out basic research, not clinical trials, and even here, it is arguable whether it necessitates the personal enrichment of investigators. Members of medical school faculties who conduct clinical trials should not accept any payments from drug companies except research support, and that support should have no strings attached, including control by drug companies over the design, interpretation, and publication of research results.
Medical schools and teaching hospitals should rigorously enforce that rule, and should not enter into deals with companies whose products members of their faculty are studying. Finally, there is seldom a legitimate reason for physicians to accept gifts from drug companies, even small ones, and they should pay for their own meetings and continuing education.
After much unfavorable publicity, medical schools and professional organizations are beginning to talk about controlling conflicts of interest, but so far the response has been tepid. They consistently refer to "potential" conflicts of interest, as though that were different from the real thing, and about disclosing and "managing" them, not about prohibiting them. In short, there seems to be a desire to eliminate the smell of corruption, while keeping the money. Breaking the dependence of the medical profession on the pharmaceutical industry will take more than appointing committees and other gestures. It will take a sharp break from an extremely lucrative pattern of behavior. But if the medical profession does not put an end to this corruption voluntarily, it will lose the confidence of the public, and the government (not just Senator Grassley) will step in and impose regulation. No one in medicine wants that.
Notes
[1]Gardiner Harris and Benedict Carey, "Researchers Fail to Reveal Full Drug Pay," The New York Times, June 8, 2008.[2]Most of the information in these paragraphs, including Nemeroff's quote in the summer of 2004, is drawn from a long letter written by Senator Grassley to James W. Wagner, President of Emory University, on October 2, 2008.
[3]See Gardiner Harris, "Leading Psychiatrist Didn't Report Drug Makers' Pay," The New York Times, October 4, 2008.
[4]Senator Grassley is current investigating Wyeth for paying a medical writing firm to ghost-write articles favorable to its hormone-replacement drug Prempro.
[5]Some of this material is drawn from my article "Industry-Sponsored Clinical Research: A Broken System," TheJournal of the American Medical Association, September 3, 2008.
[6]Justin E. Bekelman et al., "Scope and Impact of Financial Conflicts of Interest in Biomedical Research: A Systematic Review," The Journal of the American Medical Association, January 22, 2003.
[7]Eric G. Campbell et al., "Institutional Academic–Industry Relationships," The Journal of the American Medical Association, October 17, 2007.
[8]Erick H. Turner et al., "Selective Publication of Antidepressant Trials and Its Influence on Apparent Efficacy," The New England Journal of Medicine, January 17, 2008.
[9]See Wayne Kondro and Barb Sibbald, "Drug Company Experts Advised Staff to Withhold Data About SSRI Use in Children," Canadian Medical Association Journal, March 2, 2004.
[10]Irving Kirsch et al., "The Emperor's New Drugs: An Analysis of Antidepressant Medication Data Submitted to the US Food and Drug Administration," Prevention & Treatment, July 15, 2002.
[11]Rosie Taylor and Jim Giles, "Cash Interests Taint Drug Advice," Nature, October 20, 2005.
[12]David Tuller, "Seeking a Fuller Picture of Statins," The New York Times, July 20, 2004.
[13]Lisa Cosgrove et al., "Financial Ties Between DSM-IV Panel Members and the Pharmaceutical Industry," Psychotherapy and Psychosomatics, Vol. 75, No. 3 (2006).
[14]On August 4, 2008, the FDA announced that $50,000 is now the "maximum personal financial interest an advisor may have in all companies that may be affected by a particular meeting." Waivers may be granted for amounts less than that.
[15]See Petersen, Our Daily Meds, p. 224.
[16]Petersen's book is a part of a second wave of books exposing the deceptive practices of the pharmaceutical industry. The first included Katharine Greider's The Big Fix: How the Pharmaceutical Industry Rips Off American Consumers (PublicAffairs, 2003), Merrill Goozner's The $800 Million Pill: The Truth Behind the Cost of New Drugs (University of California Press, 2004), Jerome Avorn's Powerful Medicines: The Benefits, Risks, and Costs of Prescription Drugs (Knopf, 2004), John Abramson's Overdo$ed America: The Broken Promise of American Medicine (HarperCollins, 2004), and my own The Truth About the Drug Companies: How They Deceive Us and What to Do About It (Random House, 2004).
[17]See the review by Frederick Crews of Lane's book and two others, The New York Review, December 6, 2007.
[18]See Gardiner Harris and Benedict Carey, "Researchers Fail to Reveal Full Drug Pay," The New York Times, June 8, 2008.
Thursday, 22 December 2011
FOSTER CHILDREN GIVEN MORE PSYCHOTROPIC DRUGS THAN REST OF POPULATION
http://am.blogs.cnn.com/2011/12/02/study-foster-children-prescribed-more-psychotropic-drugs/
WATCH VIDEO NEWS CLIP BY CLICKING ON THE LINK ABOVE OR THE TITLE
Saturday, 17 December 2011
CONGRESSMAN RON PAUL DECEMBER 2011 - U.S. GOVERNMENT FORCES PSYCHOTROPIC DRUGS ON CHILDREN THROUGH MASS SCREENING + TAKES KIDS INTO STATE CARE IF THE PARENTS STOP GIVING THEIR OWN CHILDREN THE DRUGS DUE TO WORRIES ABOUT THE SIDE EFFECTS- CRAZY! - YOUTUBE VIDEO
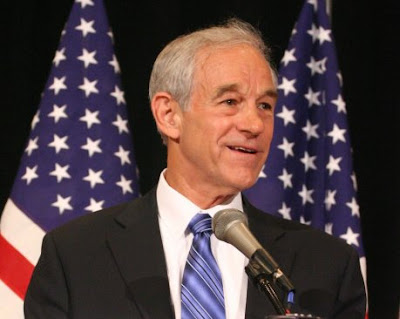 |
| CONGRESSMAN RON PAUL CHALLENGES MASS SCREENING |
http://youtu.be/SPqs4Xnbdzw
CLICK ON LINK ABOVE OR TITLE TO SEE THIS CONGRESSMAN'S CONCERN
Congressman Ron Paul has re-introduced The Parental Consent Act , A bill which prohibits federal funds from being used to establish or implement any universal or mandatory mental health, psychiatric, or socioemotional screening program.
“Many children have suffered harmful side effects from using psychotropic drugs. Some of the possible side effects include mania, violence, dependence and weight gain. Yet, parents are already being threatened with child abuse charges if they resist efforts to drug their children. Imagine how much easier it will be to drug children against their parents’ wishes if a federally-funded mental-health screener makes the recommendation.” – RON PAUL
Sign the petition in support of the Parental Consent Act here: http://www.petitiononline.com/rppca/petition.html
Bill information: The Parental Consent Act 2011 (H.R. 2769 – previously H.R. 2218 in 2009) Prohibits federal education funds from being used to pay any local educational agency or other instrument of government that uses the refusal of a parent or legal guardian to provide consent to mental health screening as the basis of a charge of child abuse, child neglect, medical neglect, or education neglect until the agency or instrument demonstrates that it is no longer using such refusal as a basis of such charges.
Defines a screening program under this Act as any mental health screening program in which a set of individuals is automatically screened without regard to whether there was a prior indication of a need for mental health treatment, including: (1) any program of state incentive grants to implement recommendations in the July 2003 report of the New Freedom Commission on Mental Health, the State Early Childhood Comprehensive System, grants for TeenScreen, and the Foundations for Learning Grants; and (2) any student mental health screening program that allows mental health screening of individuals under 18 years of age without the express, written, voluntary, informed consent of the parent or legal guardian of the individual involved.
Ron Paul speech given on April 30, 2009 on his bill, The Parental Consent Act (formerly H.R. 2218, now reintroduced as H.R. 2769 ):
Madam Speaker, I rise to introduce the Parental Consent Act. This bill forbids Federal funds from being used for any universal or mandatory mental-health screening of students without the express, written, voluntary, informed consent of their parents or legal guardians. This bill protects the fundamental right of parents to direct and control the upbringing and education of their children.
The New Freedom Commission on Mental Health has recommended that the federal and state governments work toward the implementation of a comprehensive system of mental-health screening for all Americans. The commission recommends that universal or mandatory mental-health screening first be implemented in public schools as a prelude to expanding it to the general public. However, neither the commission’s report nor any related mental-health screening proposal requires parental consent before a child is subjected to mental-health screening. Federally-funded universal or mandatory mental-health screening in schools without parental consent could lead to labeling more children as “ADD” or “hyperactive” and thus force more children to take psychotropic drugs, such as Ritalin, against their parents’ wishes.
Already, too many children are suffering from being prescribed psychotropic drugs for nothing more than children’s typical rambunctious behavior. According to Medco Health Solutions, more than 2.2 million children are receiving more than one psychotropic drug at one time. In fact, according to Medico Trends, in 2003, total spending on psychiatric drugs for children exceeded spending on antibiotics or asthma medication.
Many children have suffered harmful side effects from using psychotropic drugs. Some of the possible side effects include mania, violence, dependence, and weight gain. Yet, parents are already being threatened with child abuse charges if they resist efforts to drug their children. Imagine how much easier it will be to drug children against their parents’ wishes if a federally-funded mental-health screener makes the recommendation.
Universal or mandatory mental-health screening could also provide a justification for stigmatizing children from families that support traditional values. Even the authors of mental-health diagnosis manuals admit that mental-health diagnoses are subjective and based on social constructions. Therefore, it is all too easy for a psychiatrist to label a person’s disagreement with the psychiatrist’s political beliefs a mental disorder. For example, a federally-funded school violence prevention program lists “intolerance” as a mental problem that may lead to school violence. Because “intolerance” is often a code word for believing in traditional values, children who share their parents’ values could be labeled as having mental problems and a risk of causing violence. If the mandatory mental-health screening program applies to adults, everyone who believes in traditional values could have his or her beliefs stigmatized as a sign of a mental disorder. Taxpayer dollars should not support programs that may label those who adhere to traditional values as having a “mental disorder.”
Madam Speaker, universal or mandatory mental-health screening threatens to undermine parents’ right to raise their children as the parents see fit. Forced mental-health screening could also endanger the health of children by leading to more children being improperly placed on psychotropic drugs, such as Ritalin, or stigmatized as “mentally ill” or a risk of causing violence because they adhere to traditional values. Congress has a responsibility to the nation’s parents and children to stop this from happening. I, therefore, urge my colleagues to cosponsor the Parental Consent Act.
For more information on the Parental Consent Act watch this video featuring Kent Snyder, Ron Paul’s Presidential campaign manager 2008, and former Executive Director of the Liberty Committee http://www.cchrint.org/videos/experts/ron-pauls-parental-consent-act-of-2009/
BE WARY OF THE SCIENTIFIC RATIONALIST MORAL ARGUMENTS - COURTESY OF SCIENTIFIC AMERICAN BLOG - "The best lack all conviction, while the worst are full of passionate intensity." But if we all become zealots, we’re really in trouble.
http://blogs.scientificamerican.com/cross-check/2010/10/11/be-wary-of-the-righteous-rationalist-we-should-reject-sam-harriss-claim-that-science-can-be-a-moral-guidepost/
"Be wary of the righteous rationalist: We should reject Sam Harris’s claim that science can be a moral guidepost."
By John Horgan | October 11, 2010 |
Say what you will about Sam Harris, the man’s got guts. In The End of Faith (W. W. Norton, 2005) and Letter to a Christian Nation (Knopf, 2006), Harris, a neuroscientist, rejects the notion that science and religion can coexist. We can’t believe in science, Harris says, and still believe in supernatural beings that part seas, resurrect dead people and keep tabs on our naughtiness and niceness.
Harris slams nonbelieving apologists for religion such as the late biologist Stephen Jay Gould. With typical rhetorical grandiosity, Gould proposed that science and religion need not conflict because they are "nonoverlapping magisteria" that address separate realms of existence. Science tells us what is, religion what should be. Given all the crimes committed in religion’s name, Harris retorts, why would anyone look to it for moral guidance?
I’m with Harris up to this point. I part company with him when he argues in his new book The Moral Landscape (Free Press, 2010)—which comes fortified with blurbs from Steven Pinker, Richard Dawkins and other antireligious scientific luminaries—that science can take religion’s place as the supreme arbiter of moral "truth". "There are right and wrong answers to moral questions," Harris asserts, "just as there are right and wrong answers to questions of physics." Questions about morality, he explains, are really questions about human happiness or "well-being," and these questions can be empirically resolved, just as questions about diet and disease can be.
One can raise all sorts of philosophical objections to this position, and the philosopher Kwame Anthony Appiah does just that in a New York Times review ironically titled "Science Knows Best". My concerns about Harris’s proposal are simpler: I just look at the harm—historical and recent—wreaked by scientists supposedly concerned with humanity’s well-being. Some examples:
—From 1946 to 1948, physicians funded by the National Institutes of Health deliberately infected nearly 700 Guatemalan prisoners, mental-hospital patients and soldiers with syphilis to test their responses to antibiotics. The leader of this research, John C. Cutler, was also involved in the infamous Tuskegee studies, in which scientists withheld antibiotics from black American males naturally infected with syphilis. "It’s ironic—no, it’s worse than that, it’s appalling—that, at the same time as the United States was prosecuting Nazi doctors for crimes against humanity, the U.S. government was supporting research that placed human subjects at enormous risk," the bioethicist Mark Siegler told The New York Times.
—In the 1950s and 1960s researchers at leading universities embedded electrodes in the brains of mental patients to test whether minds and bodies can be manipulated via electrical stimulation of neural tissue. In 1969 the Yale physiologist Jose Delgado (whom I profiled in Scientific American in 2005), extolled the benefits of brain implants in his book Physical Control of the Mind: Toward a Psychocivilized Society (Harper & Row, 1971). Delgado declared that brain implants could help create "a less cruel, happier and better man." In 1970 Frank Ervin and Vernon Mark, two brain-implant researchers at Harvard University with whom Delgado had collaborated, proposed in their book Violence and the Brain (HarperCollins, 1970) that brain implants and psychosurgery might quell violent crime and rioting in inner cities.
—In recent decades prescriptions of drugs for children, including infants, supposedly suffering from psychiatric illness have skyrocketed. Some 500,000 U.S. children and adolescents are now taking antipsychotic drugs, Duff Wilson reported recently in The New York Times, even though some experts believe the drugs "may pose grave risks to development of both their fast-growing brains and their bodies." In another Times article Wilson details how psychiatrists who tout the benefits of antipsychotics receive grants, vacations, meals and other gifts from drug manufacturers. The Harvard physician Joseph Biederman, whose research helped spur a 40-fold increase in diagnoses of bipolar disorders in children between 1994 and 2003, received $1.6 million, "from companies including makers of antipsychotic drugs prescribed for some children who might have bipolar disorder," according to Wilson.
Some will complain that it is unfair to hold science accountable for the misdeeds of a minority. It is not only fair, it is essential, especially when scientists as prominent as Harris are talking about creating a universal, scientifically validated morality. Moreover, Harris blames Islam and Catholicism for the actions of suicide bombers and pedophilic priests, so why should science be exempt from this same treatment?
Clearly, some bad scientists are just greedy opportunists who care about only their own well-being. But those who fervently believe their own rhetoric about saving humanity may be even more dangerous. Consider the harm done in the name of Marxism and eugenics, pseudoscientific (not religious) ideologies that inspired two of the most lethal regimes in history—Stalin’s U.S.S.R. and Nazi Germany.
Harris asserts in Moral Landscape that ignorance and humility are inversely proportional to each other; whereas religious know-nothings are often arrogant, scientists tend to be humble, because they know enough to know their limitations. "Arrogance is about as common at a scientific conference as nudity," Harris states. Yet he is anything but humble in his opus. He castigates not only religious believers but even nonbelieving scientists and philosophers who don’t share his hostility toward religion.
Harris further shows his arrogance when he claims that neuroscience, his own field, is best positioned to help us achieve a universal morality. "The more we understand ourselves at the level of the brain, the more we will see that there are right and wrong answers to questions of human values." Neuroscience can’t even tell me how I can know the big, black, hairy thing on my couch is my dog Merlin. And we’re going to trust neuroscience to tell us how we should resolve debates over the morality of abortion, euthanasia and armed intervention in other nations’ affairs?
I suspect Harris wants to rely on brain scans to measure "well-being" because he doesn’t trust people to simply say what makes them happy. If a Muslim girl says that she likes wearing a veil, as many do, she doesn’t know what’s good for her, Harris might say. Maybe she doesn’t, but magnetic resonance imaging won’t help us resolve these sorts of issues.
When scientists venture into the moral realm, they should not claim that their investigations of what is yield special insights into what should be. I realize I’m asking a lot of scientists—and secularists—to be humble when religious and political zealots like Glenn Beck and Sarah Palin are so bloated with self-righteousness. This asymmetry recalls Yeats’s famous line from his poem "The Second Coming": "The best lack all conviction, while the worst are full of passionate intensity." But if we all become zealots, we’re really in trouble.
Subscribe to:
Comments (Atom)






















